The risk prediction tool, developed by the Melanoma Institute Australia, has been validated in a large, international cohort of patients.
A sentinel node metastasis risk predictor originally developed in Australia has been found to be a robust and precise model when tested internationally.
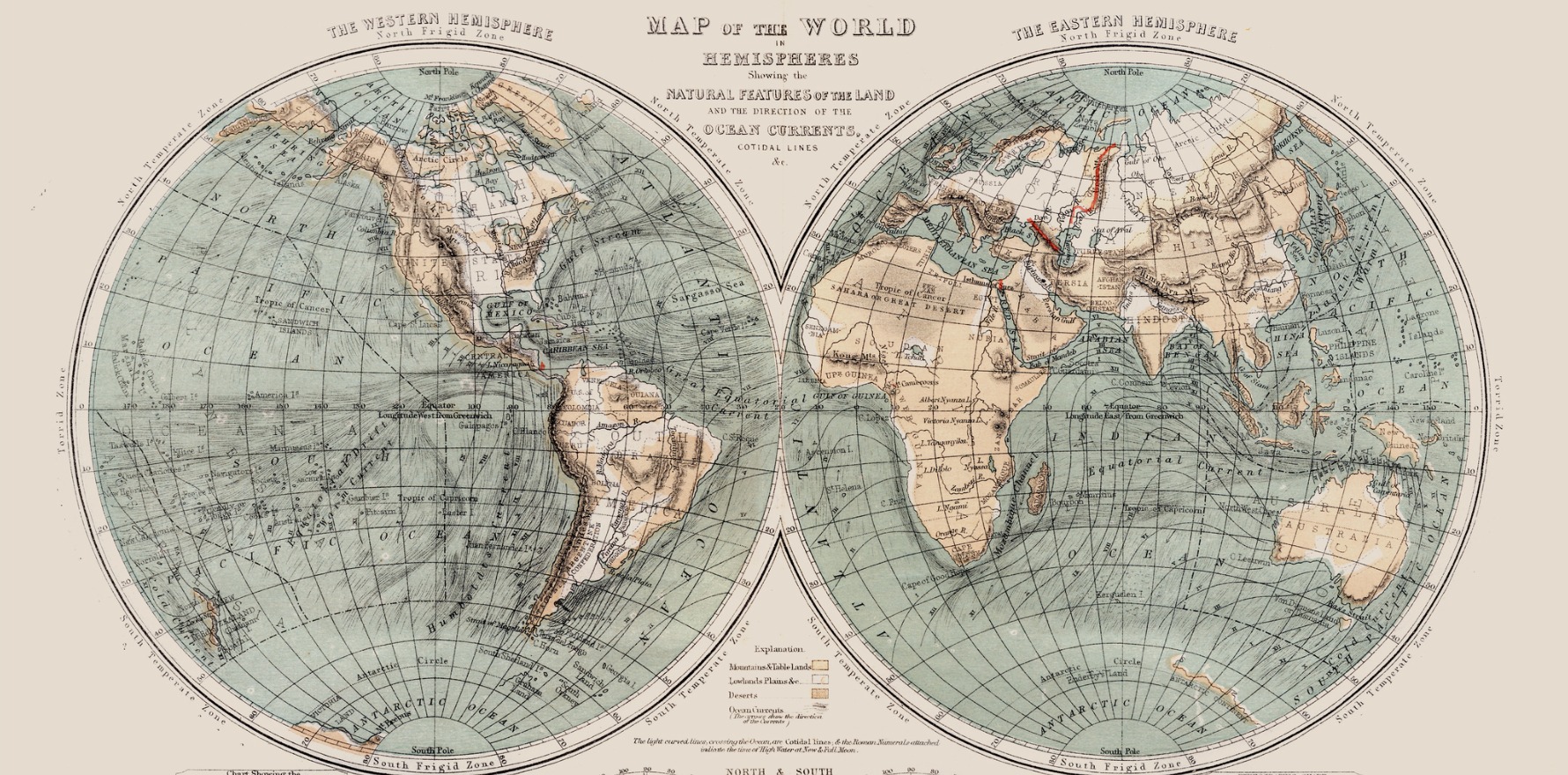
Launched in 2020, the Melanoma Institute Australia’s sentinel node metastasis risk prediction tool has been used by clinicians in more than 30 different countries to estimate the risk of sentinel node positivity in patients with primary cutaneous melanoma. But despite its widespread use, the tool has only been validated in a handful of non-Australian populations.
Now, a new study, published in JAMA Dermatology, has further validated the risk calculator in a cohort of over 15,000 patients from Europe, North and South America and Australasia to determine the applicability of the scale on a global level.
“We knew the importance of validating the tool in an external population back when we were building the tool,” said senior author Associate Professor Alexander Varey, a plastic and reconstructive surgeon from the Melanoma Institute Australia.
“So, we got our long-time collaborators from MD Anderson to provide us with data to validate it in our first publication.
“But at the same time, when I started speaking to some of my friends and colleagues around the world, they highlighted that the tool hadn’t been validated in their populations. We thought this was a really fair point, so we set out trying to recruit other sites to be able to do a second validation study.”
Six parameters can be entered into the risk calculator, including age, Breslow thickness and melanoma subtype (mandatory), and tumour mitotic rate, the presence of ulceration and lymphovascular invasion (optional). The calculator uses eight different statistical models to determine risk based on the specific combination of mandatory and optional parameters available.
Twenty percent of patients in the current cohort had data available for all six parameters; the remaining 80% of the cohort were missing data at least one of the three optional parameters.
The area under the receiver operator characteristics curve (AUC) for the subset of patients with complete data was 73% (95% confidence interval 70.6%-75.3%), where 50% indicates the test is no better than chance at estimating metastasis risk and 100% indicates the test has perfect sensitivity and specificity.
This performance was almost identical to the performance in the original Australian development cohort, where the AUC was 73.9%, thereby confirming its accuracy.
Professor Varey said he was reassured by the consistency of the findings between the original and newer validation analyses.
“You never know what you’re going to get when you get into the research, so it was good to see the tool was performing consistently across different populations around the world,” he told Oncology Republic.
Related
Similar AUC values were found in the limited data models when one (70.8%, 95% CI 68.1%-72.7%), two (71.5%, 68.1%-75.8%) or three (70.1%, 61.4%-83.5%) of the optional parameters were missing.
The online tool has already been updated to include the revised confidence intervals around the point estimate of melanoma risk.
Professor Varey highlighted that while further validation in other populations was always a possibility, another future research direction was comparing the clinical and cost-effectiveness of the risk prediction tool against novel gene expression profiles being developed by various biotechnology companies.