Experts hope the new framework will lead to better detection and outcomes in people living with HIV.
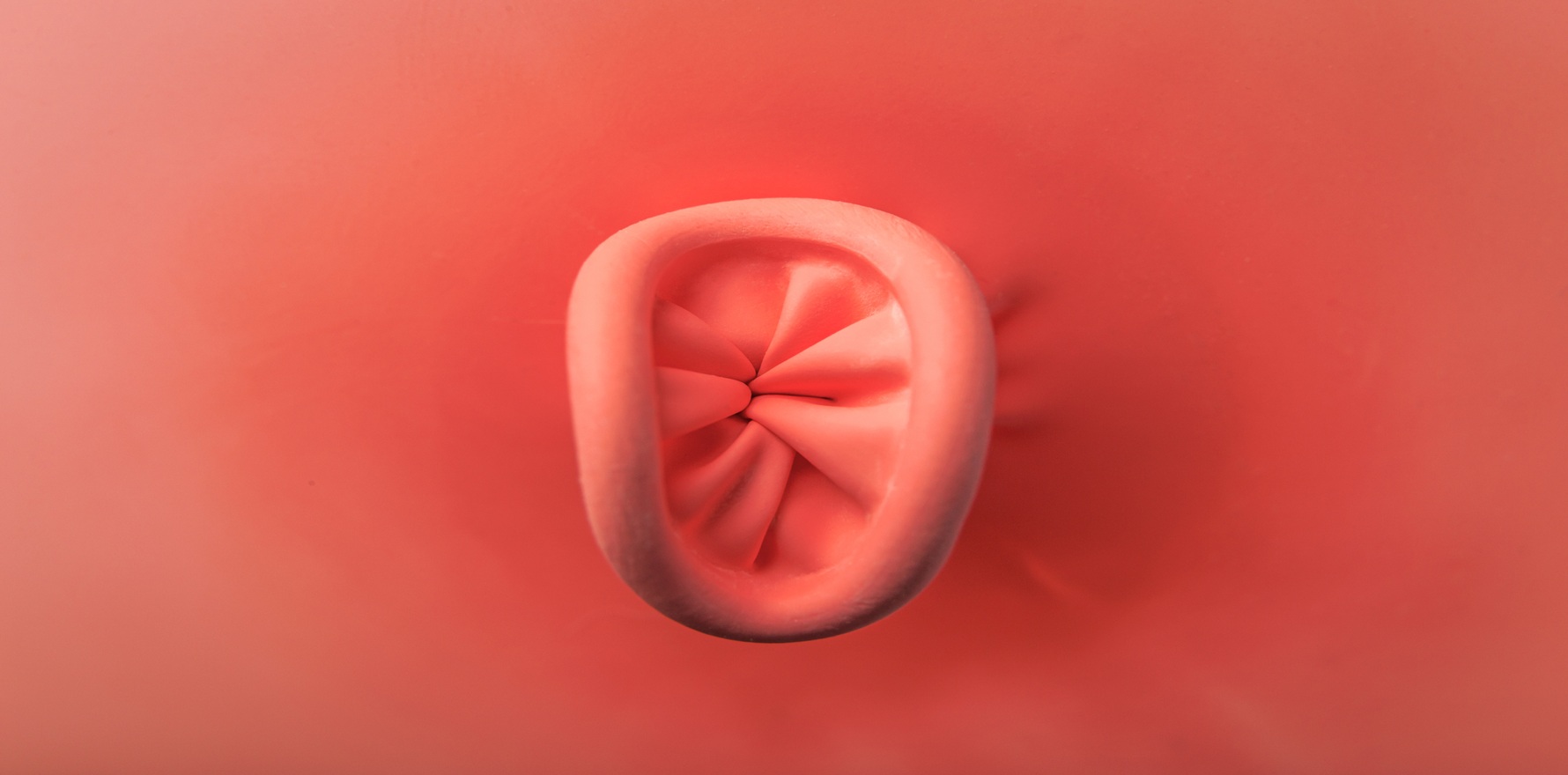
The Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) has launched the country’s first national anal cancer screening guidelines for people living with HIV.
Professor Jason Ong, a Melbourne-based sexual health physician and researcher, said evidence-based screening was essential to lower the anal cancer incidence rate in men who have sex with men who are living which HIV, which is more than 60 times higher than the general population.
“Currently, anal squamous cell cancer is often diagnosed at an advanced stage due to a lack of obvious early-state symptoms. These guidelines advocate for proactive screening to drive earlier detection and a better prognosis for patients,” the ASHM vice president said in a statement.
“These guidelines equip healthcare providers with the latest recommendations for screening, diagnosis and management of precursor lesions of anal cancer in people living with HIV – ensuring early interventions and better patient outcomes.”
The guidelines, which were developed as part of a collaboration between the ASHM, the Alfred, Douglass Hanly Moir Pathology, Monash University, the National Association of People with HIV Australia and the Kirby Institute, among others, cover possible anal cancer screening methods, screening intervals and cessation and the management of screening test results. Five key recommendations are made across these areas.
Specifically, gay, bisexual and other men who have sex with men (GBM) and trans women living with HIV over the age of 35 as well as cis women, trans men and other cis men (not GBM) who live with HIV over the age of 45 should also be offered primary high-risk human papillomavirus testing with cytology triage every three years for those who are negative for HRHPV.
Screening can be discontinued as part of a shared decision-making process once an individual turns 75, or in individuals who are not currently sexually active and have two consecutive negative test results.
Related
Dr Ong emphasised that all anal cancer screening should include an internal physical examination, screening of the perianal region and a detailed medical history that includes sexual behaviour history, other potential activities known to increase cancer risk (e.g., smoking) and other factors that may contribute to a patient’s immune system being supressed.
“Regular digital anorectal exams and anal cytology or HPV tests can detect abnormalities before they progress to cancer. Following these guidelines means saving lives through early detection,” he told media.
Almost 90% of anal cancer cases in Australia are caused by HPV. In 2024 the Australian Institute of Health and Welfare reported there were over 3000 people living with anal cancer at the end of 2020 who had been diagnosed in the preceding decade, with nearly twice as many females as males.
The anal cancer screening guidelines for people living with HIV can be accessed via the ASHM website.