A recent clinical trial confirms what has only been shown in retrospective studies, paving the way for improved patient outcomes.
Almost double the number of patients experienced mild or no erectile dysfunction after undergoing NeuroSAFE-guided nerve-sparing compared to standard robot-assisted radical prostatectomy (RARP) in a groundbreaking new study.
Using intraoperative margin assessment during prostatectomy instead of the current practice of relying of preoperative imaging to assess whether neurovascular bundles can be preserved, both sexual function and continence outcomes were significantly improved.
NeuroSAFE PROOF was amulticentre, patient-blinded, randomised, controlled phase three trialin the UK which compared NeuroSAFE to standard RARP. Until now, NeuroSAFE-guided nerve-sparing has only ever been evaluated retrospectively.
In standard RARP, it’s a ‘better safe than sorry’ situation and if preoperative imaging suggests that cancer may be present near the neurovascular bundles, there is often no choice but to remove part or all the nerves. The impairment of urinary continence and erectile function has been an unfortunate but accepted side-effect up until this point.
However, NeuroSAFE is intraoperative, meaning real-time frozen section analysis can determine whether the neurovascular bundles can be spared. Once the prostate has been removed, thin slices from the posterolateral margins can be quickly evaluated mid-surgery.
If cancer is detected near the margins, further tissue can be removed on the spot. But if it’s not detected near the bundles, they can be preserved, and surgery can be concluded.
Professor Declan Murphy, Director of Robotic Surgery at the Peter MacCallum Cancer Centre, explained that the trial participants all had good sexual function prior to surgery, which is not always the case in older men, especially those with comorbidities. The study group represents those with the highest consequence from prostatectomy in terms of sexual function, he said.
“By having this intraoperative assessment of the margin to make sure we’re not leaving cancer behind, you greatly increase the proportion of patients who are going to have nerve-sparing. This is going to benefit a whole bunch of men who are going to still get a good cancer result but also have a better chance of regaining sexual function,” he said.
Of the standard RARP group, 56% were able to have bilateral nerve-sparing, compared to 82% in the NeuroSAFE group.
Half of the 407 randomly assigned participants underwent NeuroSAFE-guided surgery, while the rest formed the standard RARP group. Patient outcomes were assessed using the International Index of Erectile Function (IIEF) and the International Consultation on Incontinence Questionnaire (ICIQ).
Those included had a diagnosis of non-metastatic prostate cancer that was deemed suitable to undergo RARP, good erectile function (scoring 22 or higher on the IIEF-5 without medical assistance) and no previous prostate cancer treatment. Participants were assessed for urinary continence at three and six months using the ICIQ and assessed at 12 months for erectile function using the IIEF-5 and the IIEF-6.
The NeuroSAFE group had significantly higher mean scores than the standard RARP group on both the IIEF-5 (12.7 vs 9.7) and the IIEF-6 (15.3 vs 11.5), indicating superior erectile function at 12 months post-op.
Their mean ICIQ score was also significantly lower at three months (2.42 vs 0.41), indicating an earlier improvement in continence for those who underwent NeuroSAFE-guided surgery than standard RARP.
Serious adverse events occurred in about 3% of the both the NeuroSAFE group and the standard RARP group, but all adverse events were postoperative complications, and no serious adverse events or deaths were attributed to the study intervention.
Related
However, there are practicality issues and logistical challenges to using NeuroSAFE guidance that are impossible to overcome, according to Professor Murphy.
NeuroSAFE requires specialised equipment and a nearby pathologist ready and waiting throughout surgery. It’s very challenging for most health systems around the world to have both of those things in place, he told OR.
“In Melbourne, for example, there are maybe 12 to 15 [private] hospitals every day performing radical prostatectomy for prostate cancer, and none of those hospitals have a pathology laboratory on site,” he said.
Intraoperative margin assessment is still a huge area of interest though, and the findings of the study are very valuable for showing that nerve-sparing and patient outcomes can be significantly improved.
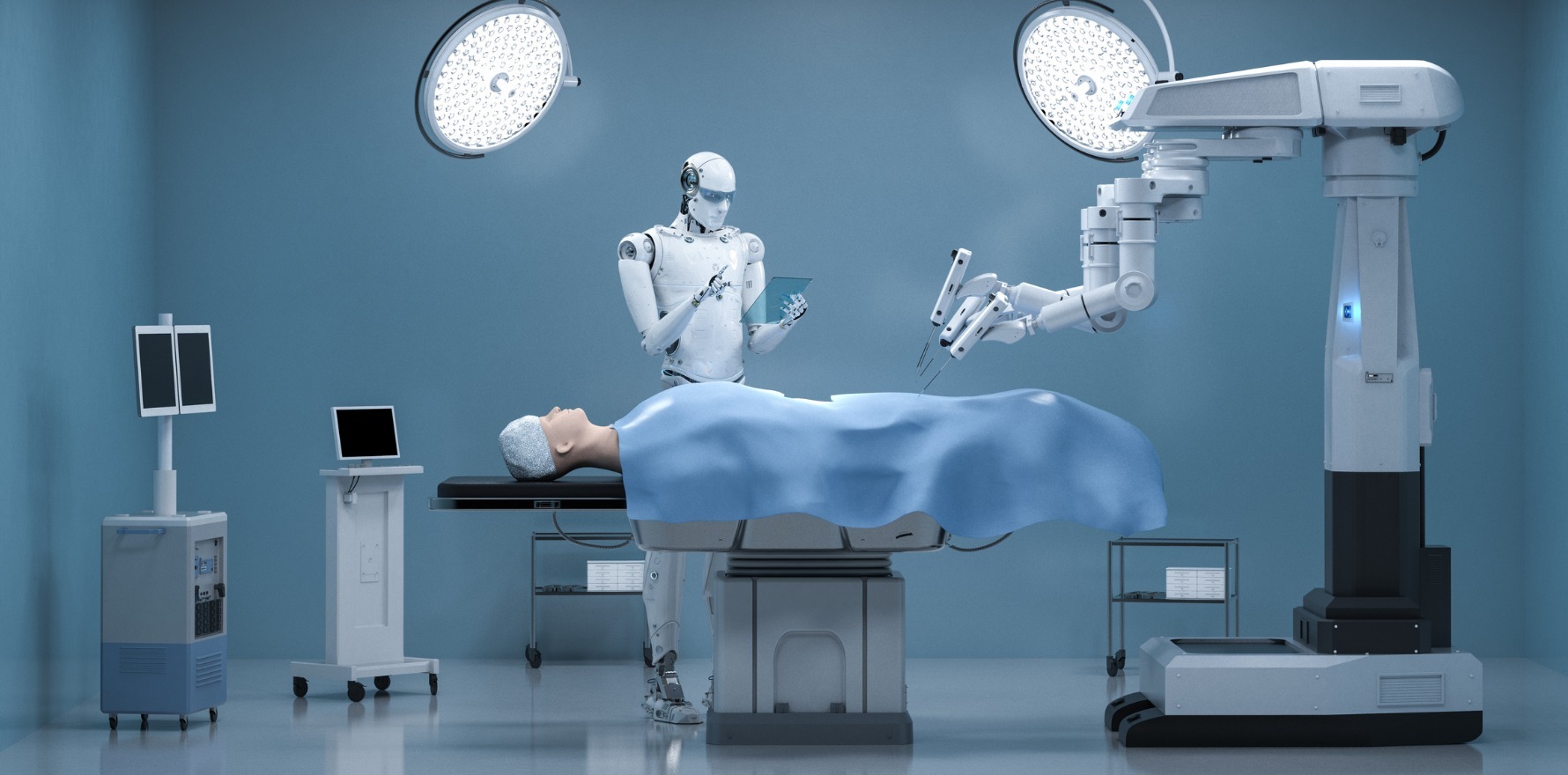
He discussed with the study authors in a recent podcast about the foundations NeuroSAFE has laid, and how technologies such as AI can build on intraoperative margin assessment.
“Using AI to assess this is already really developing legs. And what the NeuroSAFE trial has done is turbo charged that,” he told OR.
“The future is going to be using smarter visual technologies in the operating theatre, with AI assessment of the margin. And that’s really what’s got us excited.”