The gaping health inequalities exposed by the pandemic raise questions about leaders’ level of accountability.
“[Society] has placed the workers under conditions in which they can neither retain health nor live long … society knows how injurious such conditions are to the health and the life of the workers, and yet does nothing to improve these conditions. That it knows the consequences of its deeds; that its act is, therefore, not mere manslaughter, but murder.”
– Friedrich Engels, The Condition of the Working-Class in England, 18451
In the United States, a man works shoulder-to-shoulder with his unmasked colleagues in a cold, damp, meat-packing facility. He has had a fever and cough for a week, but can’t afford to skip work to go to a covid-19 testing facility.2
In Singapore, construction workers – whose work is deemed essential during a lockdown – labour at worksites that become covid-19 hotspots, then sleep in crowded dormitories with little ventilation.3
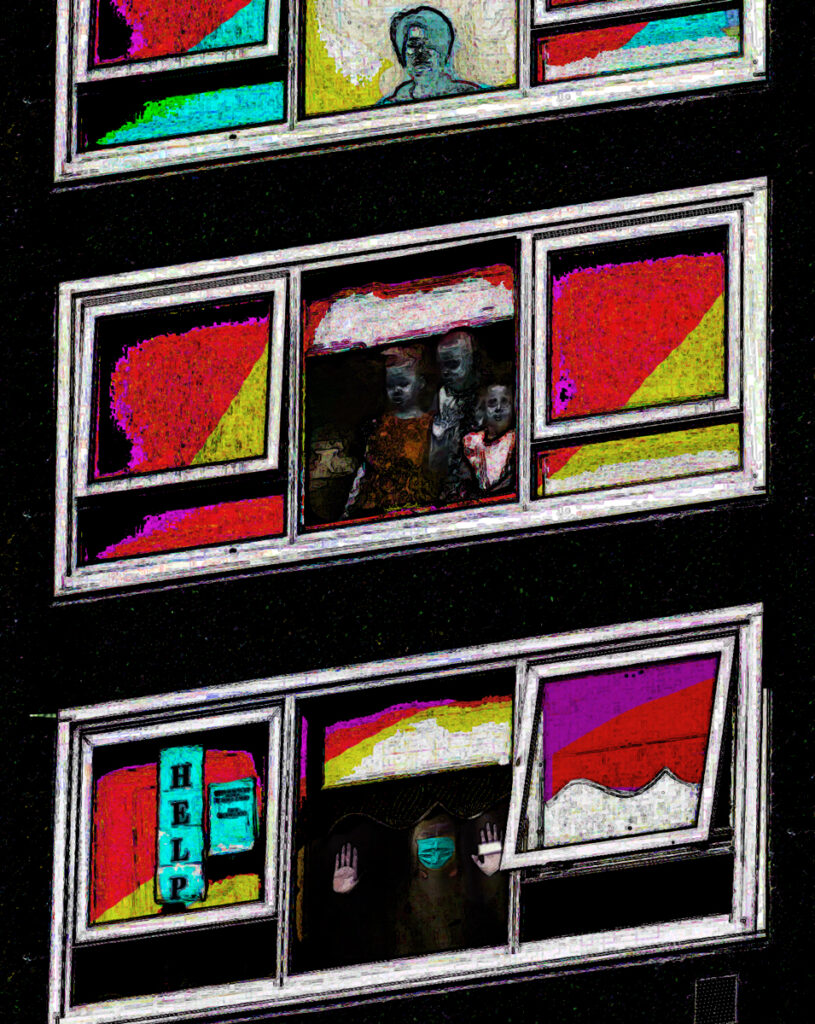
In Melbourne, 3000 residents – many from immigrant or non-English-speaking backgrounds – of nine public housing towers find themselves surrounded one afternoon by police and, without warning, are confined to their homes during a covid surge.4 They are forbidden to leave for groceries, work or exercise.
In India, a first-wave lockdown halts all public transport, abandoning workers to walk hundreds, even thousands, of kilometres back to their home towns. Hundreds are thought to have died on the way.5
In Michigan, Black people with covid but no comorbidities are 12 times more likely to die from the disease than white people.6
In high-income countries, one in four people has received a dose of covid-19 vaccine. In poorer countries, one in 500 have been vaccinated.7
“We are all in this together, for sure. But obviously we’re not all in this together equally.”
Professor Steve Tombs
In the mid-1800s, German philosopher Friedrich Engels coined the term “social murder” after witnessing the appalling conditions in which the English working class lived.
When someone inflicts bodily injury on another person, knowing that injury will be fatal, it is called murder, Engels reasoned. Yet when society deprives people of the “necessaries of life”, forcing them “through the strong arm of the law” to live in such conditions, knowing that these people will die early because of those conditions, “its deed is murder just as surely as the deed of the single individual”. It is, he wrote, “quite as much a death by violence as that by the sword or bullet.”
Rarely, if ever, has the tragedy of Engel’s social murder been writ so large as during the covid-19 pandemic.
In the United Kingdom, two professors of criminology saw parallels between the offences of omission that Engels highlighted, and what they described in a letter to The Guardian8 as “the systemic indifference and collective incompetence” of Boris Johnson’s government.
Professor Joe Sim, from Liverpool John Moores University, and Professor Steve Tombs,9 from the Open University, argued that many of the more than 100,000 deaths from covid-19 in the UK were avoidable: the result of sections of the population being forced into conditions that contributed to their premature deaths from the disease.
“People were put in a position that others in power knew there were dangers, knew that there was a possibility their lives might end prematurely, but didn’t do anything about it,” Professor Tombs says. He and Professor Sim believe that this is exactly what Engels had in mind with his crime of social murder.
While Professor Tombs acknowledges that the term is a “bit of a hammer over the head”, it’s an accessible shorthand for a collection of concepts, including structural violence, social harm and systemic institutionalised indifference towards certain individuals.
Who are those individuals? A cursory glance at local, national and international covid-19 mortality statistics leads to one immediate and obvious conclusion: Black, Asian and minority ethnic individuals are significantly over-represented in infection, hospitalisation and mortality figures among Western nations.10
Globally, the pandemic has had a more devastating effect in areas with greater income inequality.11 In places like the US, this is even more evident in areas with a higher proportion of non-white individuals.12 “We are all in this together, for sure,” Professor Tombs says. “But obviously we’re not all in this together equally.”
There are very few biological or genetic differences that might explain why non-white individuals in Western countries have fared worse than white individuals, says Dr Kumanan Rasanathan, a public health physician and unit head of Equity and Health at the World Health Organisation. These health inequities are the result of “unfair, or unjust, avoidable, and remediable differences in health between different population groups”.
“If you measure health inequities over time, you see that they change, which again shows that they’re not ‘natural’, that they are avoidable, and there is something you can do about them,” Dr Rasanathan says.
Socially determined health
The smoking gun in Engels’ social murder was the “conditions in which [workers] can neither retain health nor live long”. More recently, the term “social determinants of health” has come to encompass those conditions that directly or indirectly limit health and life for certain groups.13 These determinants include the social gradient (socioeconomic position or class), stress, social exclusion, work, social support, food and transport.
In his pivotal report on health inequalities in the UK in 2010 – the Marmot Review – epidemiologist and public health expert Professor Sir Michael Marmot said in his opening paragraph that socioeconomic position and health were fundamentally linked: “[T]he more favoured people are, socially and economically, the better their health,” he wrote.14
“So close is the link between particular social and economic features of society and the distribution of health among the population, that the magnitude of health inequalities is a good marker of progress towards creating a fairer society.” For example, those of high income live on average six years longer than those of low income, and their disability-free life expectancy is 13 years longer.
Unfortunately, income inequality has worsened, not improved, since Professor Marmot’s report. And so, therefore, has health inequality.
On the 10-year anniversary of the Marmot Review, Dr Rasanathan wrote a reflection on what had changed in the intervening decade and concluded that social injustice was still killing on a grand scale. And that was before covid-19 struck.
“It’s not surprising to me, firstly, that an event like a pandemic would exploit these inequalities and social determinants and make health inequities worse,” Dr Rasanathan says. “However, I think all of us seeing finally a pandemic have been stunned and shocked by such gross impacts on society, and the fact that it has played out in such an unequal world.”
One area where these gross impacts have been particularly evident is in employment.
Professor Ruqaiijah Yearby is a specialist in disparities in health care at the Center for Health Law Studies at Saint Louis University in Missouri, with a particular interest in how employment affects health inequity. The pandemic has provided far too many examples of how employment circumstances have put people – especially low-paid, disenfranchised workers – directly in harm’s way.
“The failure to provide everybody who is deemed an essential worker with masks or personal protective gear is key,” Professor Yearby says. This included everyone from nurses and aged care staff to meat-packing workers and farm labourers. For example, some farm workers were charged $8 by their employer for a face mask, and only given them for free after most workers on the site were infected.
Another issue was that, in the United States, infections were not tracked in many workplaces, particularly those deemed essential, such as aged care facilities and meat processing plants.
“Governments – federal and state level – made a decision that these nursing homes did not have to track the infections of their employees, I think in part because there was a worry about business liability,” Professor Yearby says.
These and other industries also weren’t required to test workers when there was an outbreak, or even inform them. In some cases, workers only found out about a hotspot in their workplace when it was reported on the local news. “You cannot stop the spread of the virus if you’re saying ‘the only people out are essential workers, but we’re not going to contact-trace and figure out whether they actually are infected’,” she says.
In Australia, essential workers largely received better protections than in the United States and many other parts of the world. But those protections didn’t extend down the supply chains that kept Australians equipped with food, clothing and consumer goods throughout the pandemic. Those supply chains often included facilities in low and middle-income countries, where workers working for big-name Australian brands were given none of the protections afforded their colleagues within Australia’s borders.
This represented – and has long done so – a major human rights issue, says Thulsi Narayanasamy, senior labour rights researcher at the Business and Human Rights Resource Centre, who has been based in Melbourne during the pandemic.
“Businesses have a responsibility to protect workers in their supply chain, and they entirely failed in providing that protection for workers on farms and in factories, who had to continue going to work,” Ms Narayanasamy says. “What it really showed for us is there was a lack of accountability or systems in place in order to hold businesses accountable for the lack of protective measures within workplaces and supply chains.”
In wealthier countries with social support networks, workers might have had the choice of not going to work, or working from home. However these were workplaces in communities and countries where the fear of hunger outweighed workers’ fear of covid-19.
In factories in Sri Lanka, the disease tore through garment workers working in close proximity without any PPE or safety provisions, Ms Narayanasamy says. Public health responses in those countries entirely failed to account for the essential workers at the bottom of the economic pecking order, who were expected to keep working in the same conditions because those further up the ladder needed them to.
“It was just so evident in the public health response that we live in a stratified society where some people’s lives are worth protecting and other people – it’s not even that they’re not worth protecting, they’re literally forgotten about in the public health response,” Ms Narayanasamy says.
People working in the human rights space have to have strong emotional constitutions in this inequal world. But even experts such as Ms Narayanasamy have been rocked by the sheer brutality of the neglect on display. The Indian workers abandoned when their government locked down the public transport network to contain the spread of covid-19 were stranded far from home with no option but to walk thousands of kilometres in the heat, dust and hunger.
“Those images that we saw, I will never get them out of my mind as long as I live.”
Structural racism
When Engels wrote his treatise, he made no mention of race. However, Professor Marmot listed race and ethnicity alongside education, occupation, income and gender as factors that influenced social position, which in turn influenced health equity or inequity.15
Professor Steffie Woolhandler, professor in urban public health at the City University of New York, says 400 years of racism and genocide, 40 years of neoliberalism, and four years of President Donald Trump set the stage for the inadequacies of public health that resulted in the United States exceeding all other G7 countries in infection and death rates from covid-19.
“Stoking racism and xenophobia is really toxic in the US environment,” Professor Woolhandler says. It’s politics that misleads low-income white people into believing that public services mean their tax dollars paying to help someone else – immigrants or people of colour – not themselves.
And few politicians have been as toxic as President Trump on this. In an eviscerating 50-page report commissioned by The Lancet, Professor Woolhandler and an international team of health, law and social policy experts categorised actions by Trump and his government – building on decades and centuries of inequality and systemic racism – that they said led to an additional 160,000 American deaths during the pandemic.16 These actions included denying refuge to migrants, undermining health coverage, weakening food assistance programs, and shifting resources from social programs to military spending or tax breaks for business.
The Hispanic community in the US was particularly hard-hit by covid-19. Hispanic Americans are traditionally a group that have better life expectancy than white Americans, despite having higher levels of poverty. This is partly attributed to the “healthy immigrant” effect: “First-generation folks tend to be healthy because they had the wherewithal to emigrate, and only healthier family members tend to emigrate,” Professor Woolhandler says. Hispanic families are also more likely to eat together at home, which is associated with better overall health.
Yet in the pandemic, the rate of infections has been twice as high in Hispanic or Latino people than in white, hospitalisation rates are three times higher, and death rates are 2.3-time higher.17
The reason, Professor Woolhandler says, is that this community has been denied access to life-saving services, both before and during the pandemic. Even if they are in the country legally, immigrants aren’t allowed to apply for food stamps or welfare for five years.
Then President Trump doubled down. “Even if it’s after five years, and they’re allowed to do it, Trump put a new rule in place that if you use food stamps or welfare, or food stamps for health insurance, you could be denied an upgrade to your immigration status,” Professor Woolhandler says.
“When you went to get a green card, if they found you used health or nutrition services, you could lose the opportunity to get a green card, you could even be reported because you wouldn’t be a citizen.”
President Trump also made it illegal for immigrants to use housing assistance, compounding the inequalities that already see Hispanic families living in crowded situations.
Furthermore, Hispanic Americans are often working in low-paid, public-facing jobs that were deemed essential during the pandemic. “Their incomes are so low that they cannot stay home, even if it’s a life-threatening situation; the boss tells them they have to go to the grocery store and unload groceries, they are too economically precarious, often, to turn them down.”
Structural racism has subtly – and not-so-subtly – influenced labour laws and regulation in the US to ensure that people of colour have been denied many of the rights and protections gained for white workers, Professor Yearby says. For example, many nursing home and hospitality workers – who are often people of colour – are labelled as independent contractors so they are not eligible for the federally-mandated minimum wage or overtime. And when paid sick leave was achieved through union negotiations, at that time people of colour weren’t allowed to join unions.
“That’s what structural racism is, we set it to be unequal,” Professor Yearby says. “Those are the people who are essential and so those are the people who we need to guarantee that they have these benefits.”
Held to account
The Lancet has accused former president Trump of the social murder of 160,000 of his citizens. More than one million Brazilian medical professionals, along with a large number of Brazilian social and union organisations, have gone a step further. In July 2020, they asked the International Criminal Court to investigate Brazil’s President Jair Bolsonaro for crimes against humanity over his mishandling of the pandemic.18
Associate Professor Douglas Guilfoyle, an expert in international and security law at UNSW Canberra, says the case is unlikely to succeed, because international governance focuses on what states do, not individuals. Also, the law in general is reluctant to impose criminal punishments for negligence.
“You punish people because of their own fault – you don’t treat them as a means to an end,” Professor Guilfoyle says. “If you punish someone for falling short of an objective standard – for example, you shall not incompetently administer a public health system – that is in a sense punishing someone to maintain some incentive for rulers to behave a particular way.”
A different approach might be to ask whether President Bolsonaro’s actions amount to a violation of human rights – for example, the right to health. But even this would be challenging to prove and gain some kind of conviction for, because how could one argue that a government’s duty was to ensure that none of its citizens would die during a pandemic?
“The core of a crime against humanity is that you need a widespread and systematic attack against a civilian population, and that attack has to be carried out by one of a list of means specified in the ICC statute,” Professor Guilfoyle says. “Negligently inflicting circumstances of life likely to lead to the destruction of a population in whole or in part is not within that list.”*
While governments and political leaders might be difficult to get in the dock, CEOs and managing directors are less so. Already, a host of civil suits are under way all across the world, trying to hold corporates to account for excess deaths that are alleged to be the result of their negligence.
In Australia, lawyers have filed class actions against aged care providers Anglicare – operator of Newmarch House – and Heritage Care, which runs Epping Gardens in Victoria. Both facilities experienced significant covid-19 outbreaks, which affected both residents and staff, although both cases are brought on behalf of families of residents, not staff. One case specifically mentions the inadequate provision of PPE to workers.19
In the US, the family of a Walmart employee who died of covid-19 is suing the company for its failure to provide PPE and properly clean the store. McDonalds and Celebrity Cruises are facing similar lawsuits over lack of PPE for staff.20 As of January 2021, more than 770 cases have been filed in US courts alone alleging companies’ mishandling of covid-19 in their workplaces.21
Professor Yearby says that under occupational health and safety laws, companies are required to report injuries and deaths of workers on the job. But there are loopholes. For example, some companies have claimed that as it wasn’t clear where a worker contracted covid-19, they may have got infected outside work, and therefore it wasn’t the company’s responsibility.
Here again, President Trump’s policies made things worse. The US Occupational Safety and Health Administration took a hands-off approach and only issued guidance – not regulation – for how companies should respond during the pandemic to protect their workers. “That’s not something an individual should or could be responsible for,” Professor Yearby says. “To me, that is one of the most glaring faults of our federal and state governments.”
Next time
“The pandemic has killed in a deeply unequal way,” says Dr Rasanathan. “Also, the measures we have put in place to contain transmission have themselves impacted socially and economically in a deeply unequal way.”
We have to learn from this, he says. With the growing threat of future pandemics, humanity cannot afford to repeat the mistakes of the past and present. “We need to have a much more proactive approach, as part of pandemic preparedness, in planning for these unequal impacts, in ensuring that we counter these inequalities.”
But the ugly face of vaccine nationalism suggests the lessons that nations and governments should be learning from the pandemic aren’t sinking in yet. “The tolerance of rich people in rich countries for the really staggering inequities that we’re seeing in access to vaccines is quite astounding,” says Associate Professor Deborah Gleeson, a public health expert at LaTrobe University.
Gleeson says the reluctance of wealthy nations to properly invest in ensuring the vaccines are allocated equitably, to invest in technology transfer and free up the intellectual property, is reminiscent of the similar recalcitrance during the HIV/AIDS epidemic in the 1990s, when millions were dying in Africa despite treatments being available.
“The measures we have put in place to contain transmission have themselves impacted socially and economically in a deeply unequal way.”
Dr Kumanan Rasanathan
There is a glimmer of hope in US President Joe Biden’s recent support of patent-waivers on covid vaccines for developing nations. However, at the time of writing, the Australian government is still holding out against it. (22)
It’s a self-defeating approach, for as long as the virus flourishes anywhere in the world, there is the risk it will spread and generate new mutations. WHO Director-General Tedros Adhanom Ghebreyesus describe vaccine inequality as a “catastrophic moral failure” on the part of wealthy nations. Engels might well have described it as social murder on a global scale.
“It’s become a cliché to say that covid has exposed much of what’s already rotten, and exposed inequalities and systematic racism, classism, sexism in societies,” says Professor Tombs. “But despite it being a cliché, it’s also true.”
After Professors Sim and Tombs published their letter in The Guardian about social murder, it was also highlighted by executive editor of the British Medical Journal Kamran Abbasi, who argued that social murder of populations was not simply a relic of a bygone age. “It is very real today, exposed and magnified by covid-19,” he wrote. “Politicians must be held to account by legal and electoral means, indeed by any national and international constitutional means necessary.”
Professor Sim says the ultimate goal is democratic accountability for the avoidable deaths that have happened as a result of these crimes of omission, neglect and negligence. But he and Professor Tombs also hope that this will lay the foundation for change.
“These global health outbreaks are going to become more common,” Professor Tombs says. “So we do need to do things better next time.”
* This quote has been amended to change ‘Deliberately’ to ‘Negligently’.
References
- https://archive.org/details/conditionworkingclassengland/page/121/mode/2up?q=social+murder
2. https://www.propublica.org/article/emails-reveal-chaos-as-meatpacking-companies-fought-health-agencies-over-covid-19-outbreaks-in-their-plants
3. https://www.sciencedirect.com/science/article/pii/S2093791121000329
4. https://www.theguardian.com/australia-news/2020/dec/17/melbourne-public-housing-covid-lockdown-violated-human-rights-victorias-ombudsman-finds
5. https://timesofindia.indiatimes.com/india/lockdown-deaths-of-those-who-never-reached-home/articleshow/75505407.cms
6. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00041-9/fulltext
7. https://news.un.org/en/story/2021/04/1089972
8. https://www.theguardian.com/world/2021/jan/27/the-failings-behind-the-uks-abysmal-death-toll
9. http://www.open.ac.uk/people/st7699
10 .https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00634-6/fulltext and https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30374-6/fulltext and https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
11. https://www.sciencedirect.com/science/article/pii/S2666776220300053?via%3Dihub and https://cepr.org/sites/default/files/CovidEconomics73.pdf
12. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768723?resultClick=1
13. https://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf
14. https://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-exec-summary-pdf.pdf
15. https://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-exec-summary-pdf.pdf
16. https://doi.org/10.1016/S0140-6736(20)32545-9
18. https://voelkerrechtsblog.org/covid-19-at-the-international-criminal-court-2/ and https://uniglobalunion.org/sites/default/files/imce/english_denuncia_presidente_icc_final.pdf
19.https://www.marsh.com/au/insights/risk-in-context/aged-care-covid-19-class-actions.html
20. https://www.business-humanrights.org/en/blog/what-are-the-avenues-for-corporate-liability-for-covid-19-related-human-rights-abuses/
21. https://btlaw.com/en/insights/publications/covid-19-related-workplace-litigation-tracker
22. https://www.theguardian.com/australia-news/2021/may/06/pressure-mounts-on-australia-to-support-covid-vaccine-intellectual-property-waiver-for-developing-nations


