Calcium can benefit your bowels as well as your bones.
Higher calcium intake is associated with a decreased risk of colorectal cancer in older adults, according to new research out of the US.
Previous research has shown that dairy products and calcium supplements can lower the risk of developing colorectal cancer, but whether the association was consistent for different sources of calcium intake and by specific tumour type was unclear.
Now, recent findings from a US longitudinal cohort study, published in JAMA Network Open, has confirmed that consuming more calcium – regardless of the source – was associated with a lower risk of colorectal cancer both overall and for specific tumour sites.
“[These findings] will raise awareness and help to provide practical, evidence-based recommendations that are easy to implement to protect against colorectal cancer risk,” said Bowel Cancer Australia spokesperson and nutritionist Joanne Wood.
“This study will help to galvanise calcium as a critical nutrient along with a diet rich in wholegrains, vegetables and fruit.”
Researchers analysed self-reported calcium intake data from over 450,000 cancer free adults aged from 50 to 71 years and followed these individuals for a median of 18 years. Calcium intake was categorised into quintiles, and colorectal cancer status was identified through probabilistic linkage with various state-based cancer registries.
After accounting for a range of sociodemographic, dietary and behavioural factors, individuals in the highest quintile for total calcium intake were 29% less likely to develop colorectal cancer compared to people in the lowest quintile for total calcium intake.
Similar associations were seen for both dietary and supplemental calcium. People in the highest dietary calcium intake quintile were 16% less likely to develop colorectal cancer compared to the lowest intake quintile, while people taking 1000mg/day or more of supplemental calcium were 20% less likely to develop colorectal cancer compared to people taking less than 400mg/day.
Related
Increased calcium intake was also associated with a lower risk of proximal colon, distal colon and rectal cancer.
People in the top quintile for total calcium intake were 25% less likely to develop proximal colon cancer compared to people in the bottom quintile, while people in the top quintile for dietary calcium intake were 13% less likely to develop cancer in their proximal colon.
People in the top quintile for total calcium intake were 27% less likely to develop distal colon cancer compared to people in the bottom quintile. An equally strong association was seen for dietary calcium intake.
Finally, people in the top quintile for total calcium intake were 39% less likely to develop rectal cancer compared to people in the bottom quintile, while people in the top quintile for supplementary calcium intake were 36% less likely to develop rectal cancer compared to the bottom 20%.
The researchers suggested two potential mechanisms that could explain the findings.
“One dairy-specific hypothesis is that calcium in dairy products binds to secondary bile acids and fatty acids in the colon, reducing their potential to promote cancer development,” they wrote.
“[Alternatively,] the WNT signalling pathway plays a crucial role in regulating cell proliferation and differentiation. The distal colon has higher WNT signalling activity, potentially making it more responsive to factors that modulate this pathway, such as calcium intake.
“Thus, enhanced cell differentiation in response to calcium could help maintain tissue integrity and reduce the risk of cancerous cell growth.”
Ms Wood agreed with the researchers regarding the potential protective mechanisms of calcium.
“Calcium binds to bile and free fatty acids in the bowel to form a protective ‘soapy’ layer. This ‘soap’ prevents bile and free fatty acid from causing damage to the lining of the colon,” she said.
An important limitation to the study is that dietary information, including calcium intake, was only assessed at one timepoint via a questionnaire – meaning the researchers were unable to assess whether changing calcium intake over time affected the association colorectal cancer.
The National Health and Medical Research Council’s Australian Dietary Guidelines recommend adults consume at least 1000mg of calcium each day.
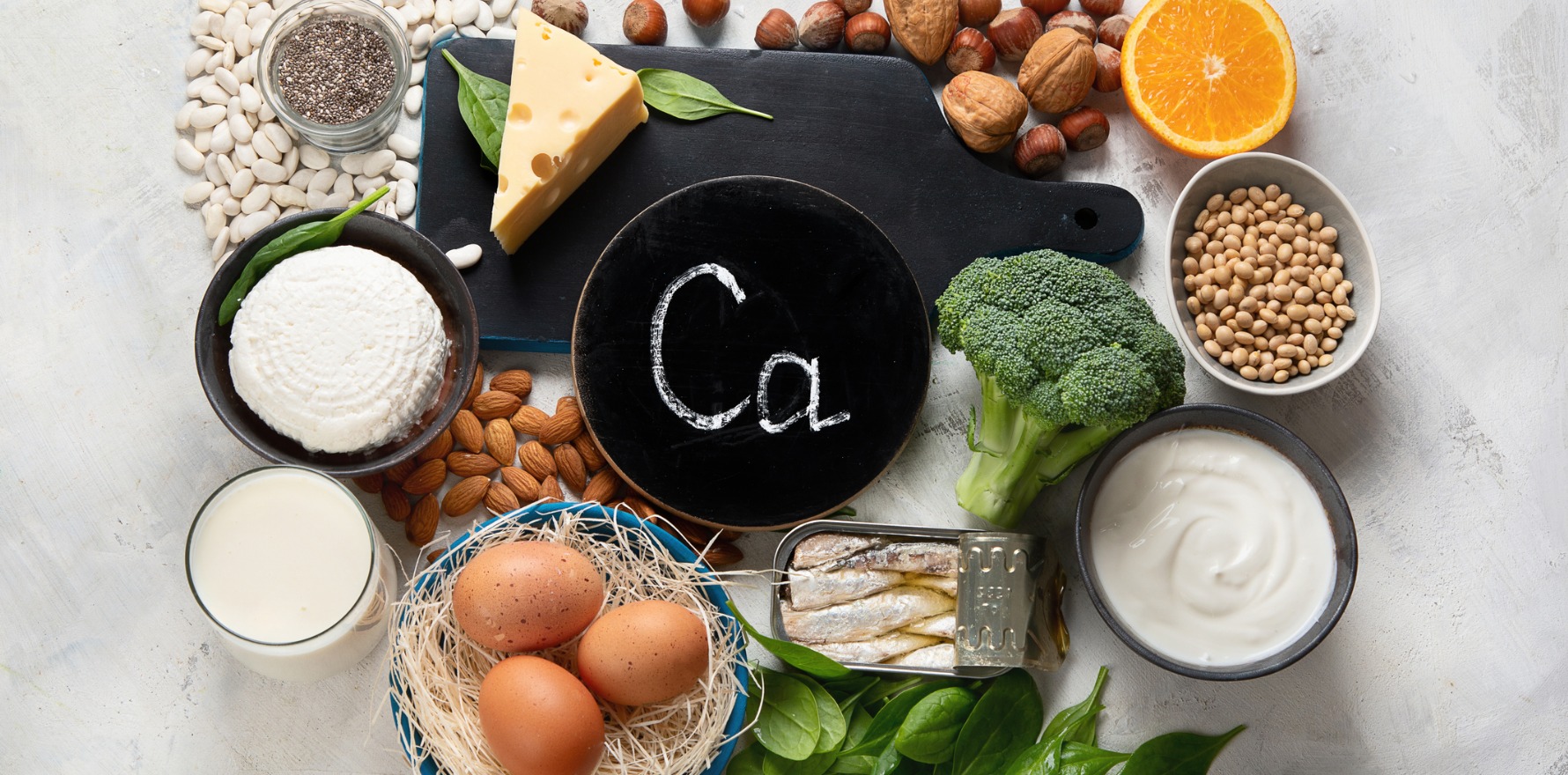
Ms Wood highlighted that individuals who are lactose intolerant or choose not to consume dairy products “can also feel confident in non-dairy calcium rich foods like sardines, green leafy vegetables, nuts and seeds, beans and legumes, fortified milk products and tofu also having a protective effect [against colorectal cancer]”.