Perth researchers say yes, and have published a new study highlighting the promising results.
Administering anti-cancer drugs at a hundred-fold lower dose than standard protocols could improve a tumour’s response to immunotherapy, Perth researchers have found.
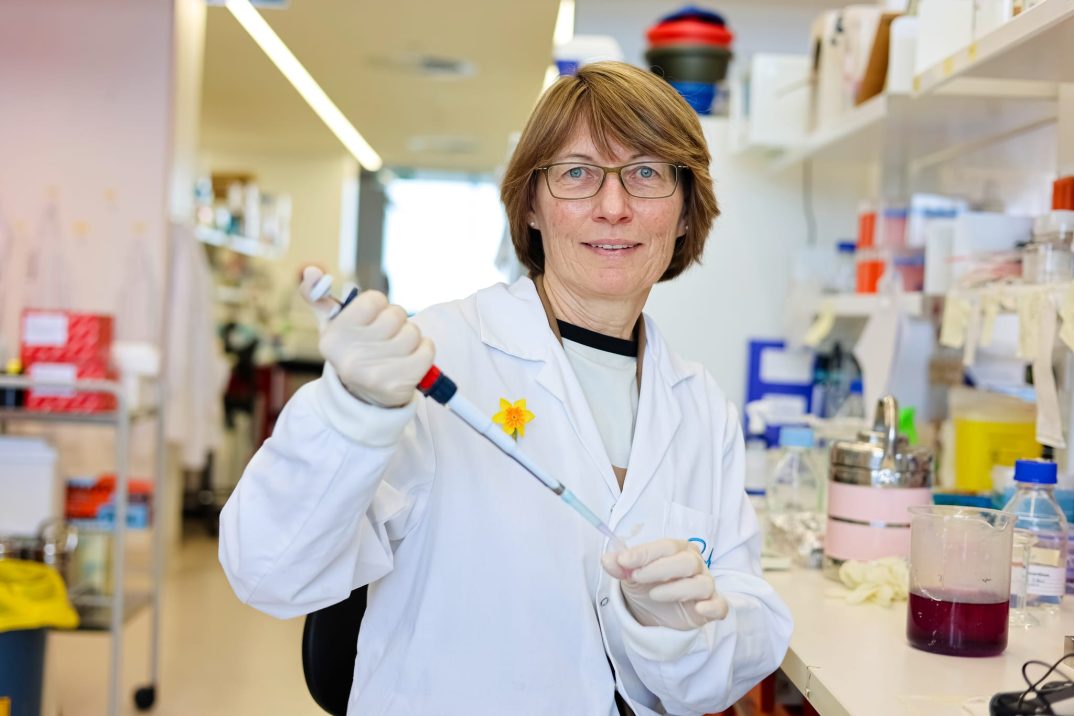
Harry Perkins Institute of Medical Research’s head of Cancer Microenvironment, Professor Ruth Ganss from The University of Western Australia (pictured below), said she was excited about the findings, which offer an alternative path to high doses of anti-cancer drugs to fight tough cancers like melanoma, brain cancer or pancreatic cancer.
“The anti-cancer drugs we are interested in are already clinically approved, this opens the way for us to propose new dosing and timing protocols for patients,” said Professor Ganss.
“Our clinical collaborators have been excited by the results that show an alternative method of administering drugs and immunotherapy together.
“The next stage in our research is a clinical trial where we will analyse tissue samples in patients with these hard-to-treat cancers.
“My team and I are excited to have found new ways of modulating cancer blood vessels with already clinically approved drugs, and now we can hopefully produce an outcome which lends itself to better, more effective treatments for the very sick and prolonging their lives.”
The research, published this week in the Journal of Clinical Investigation, showed that low-dose targeted anti-cancer therapy could durably change the tumour microenvironment without inducing adaptive resistance, creating a highly translatable pathway for redosing anti-cancer targeted therapies in combination with immunotherapy to improve outcome.
When the dose of anti-cancer drugs was considerably reduced, the tumour initially grew, but then the blood vessels surrounding the tumour normalised, allowing immunotherapy to penetrate the tumour and be more effective.
Two other researchers from the institute, Professor Jonas Nilsson, head of Melanoma Discovery, and Professor Alistair Forrest, head of Systems Biology and Genomics were among the research team, as well as scientists from the US and Germany.
“Most importantly, our data also provide a strong rationale for combining low-dose targeted therapy to induce pericyte differentiation with immunotherapy,” the authors wrote.
“In the absence of specific RGS5 small-molecule inhibitors, this study focused on targeting RGS5 signalling pathways, leading to upregulation of Rho kinase activity as well as contractile proteins. MEK/ERK and PI3K/AKT/mTOR signalling pathways are likely to regulate primal cellular responses, including survival, proliferation, and migration, in all intra-tumoral cells in a dose-dependent manner.
“However, this study focused on low-dose MEK/ERK and PI3K/AKT/mTOR pathway inhibition, which induced pericyte differentiation and overall vascular remodelling, but not cancer cell–growth inhibition.”
The researchers said it was critical to note that pericyte targeting had durable vascular effects, unlike antiangiogenic VEGF blockade, when assessed in a transgenic tumour model over an eight-week treatment course.
“Importantly, we also showed that the concept of reinstalling expression of pericyte contractile markers with low-dose drug treatment is applicable for human cancer, and indeed a high expression score of contractile markers positively correlates with melanoma patient outcomes,” they wrote.