Artificial intelligence picks up more colonic polyps and adenomas than conventional colonoscopy but is on par when it comes to finding more serious growths.
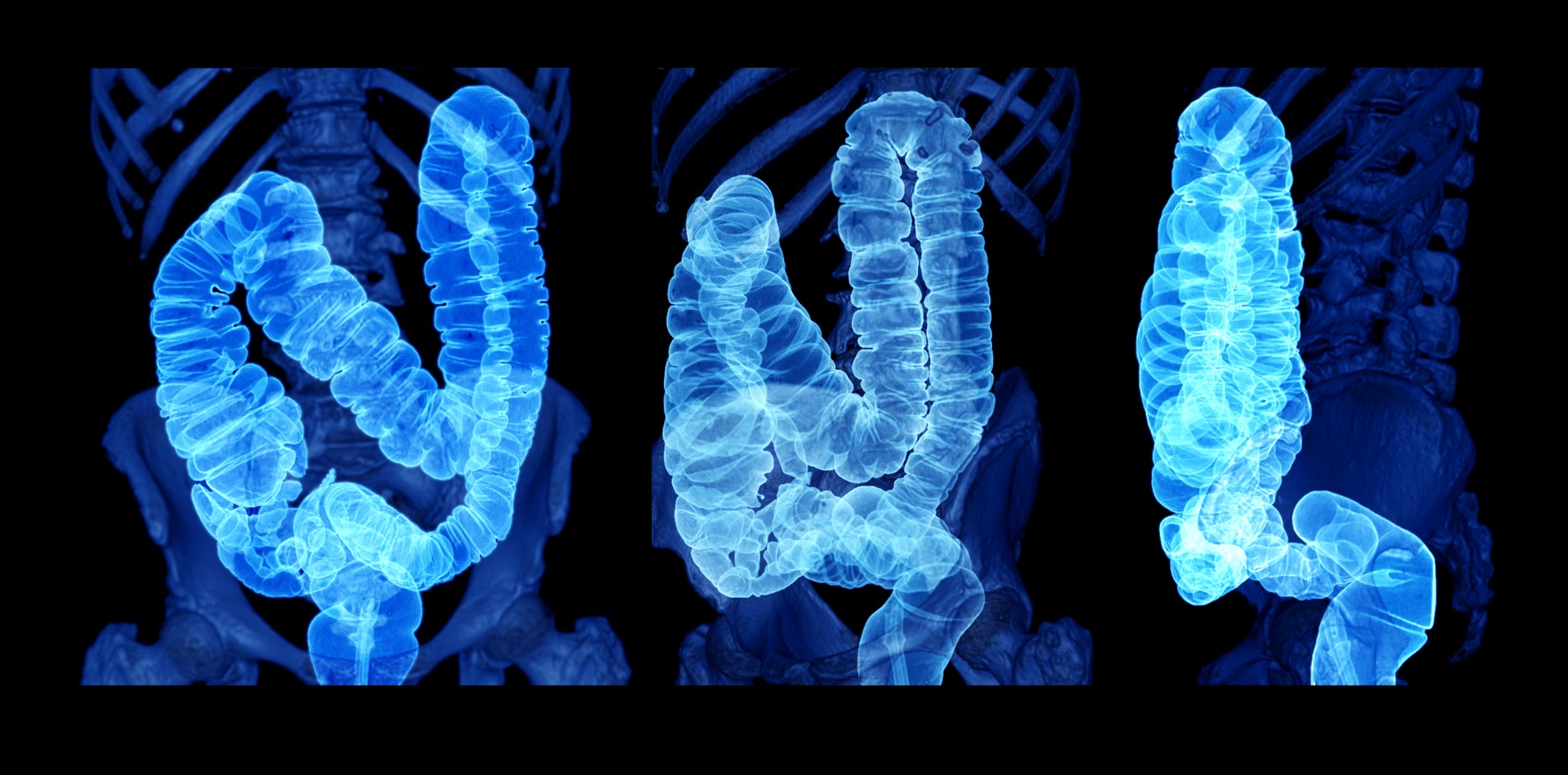
Using real-time AI during colonoscopies may increase the chances of finding pre-cancerous growths in the colon compared with conventional colonoscopy, US research suggests.
The systematic review of 44 randomised clinical trials included more than 36,000 cases and found that AI-assisted colonoscopy found more polyps and adenomas compared with conventional colonoscopy.
However, although AI-assisted colonoscopy detected marginally more serious growths than conventional colonoscopy, it was no better than the conventional method at finding serious growths per colonoscopy.
The researchers only included randomised clinical trials that used high-resolution colonoscopy equipment in patients having screening, surveillance or diagnostic colonoscopy, and looked at the average number of polyps, adenomas, advanced colonic neoplasia (CAN) and nonneoplastic polyp per colonoscopy.
They compared conventional colonoscopies with colonoscopies assisted by real-time computer-aided detection (CADe), comparing the average number of adenomas per colonoscopy and advanced colonic neoplasias (ACN) per colonoscopy for both screening methods.
Compared with conventional colonoscopy, AI-assisted colonoscopy found 35% more polyps – measured by overall polyp per colonoscopy – had a 21% higher polyp detection rate, and a 21% higher adenoma detection rate per colonoscopy.
Equivocal results were found regarding detection of advanced colonic neoplasia (ACN), with a small increase in ACN detection rate but no difference in ACN detected per colonoscopy
“For ACN, the results are mixed,” the researchers said in Annals of Internal Medicine.
“Although there is no difference in ACN per colonoscopy, there seems to be a small increase in ACN detection rate (RR = 1.16).”
They also said using CADe systems resulted in resection of almost two extra nonneoplastic polyps per 10 colonoscopies.
Some sub-groups of patients may benefit the most from computer-aided detection, such as those without a previous positive faecal immunochemical test (FIT), the researchers said.
“There may be decreased benefit in a higher proportion of patients with positive FIT results, which may indicate an attenuated benefit for the use of CADe systems for regular screening practice.”
“Future studies with focus on more important clinical outcomes, such as interval postcolonoscopy CRC, and designed with randomisation of physicians rather than patients may be considered to better evaluate the effect of these systems.”
The researchers noted that one limitation of the study was the absence of blinding.
“It is impossible to blind the endoscopists to patients’ treatment allocation in the RCTs, which could create unavoidable bias through the Hawthorne effect, as providers are aware of being observed and may explain the high ADR seen in the control groups of the included studies,” they said.
“A real-world and less controlled environment provides an opportunity to evaluate human-artificial intelligence interaction without influencing the behaviour of physicians, as evaluated in a recent meta-analysis of non-randomised studies.”